Leading scholars share insights on global leadership perspectives for a post-COVID world
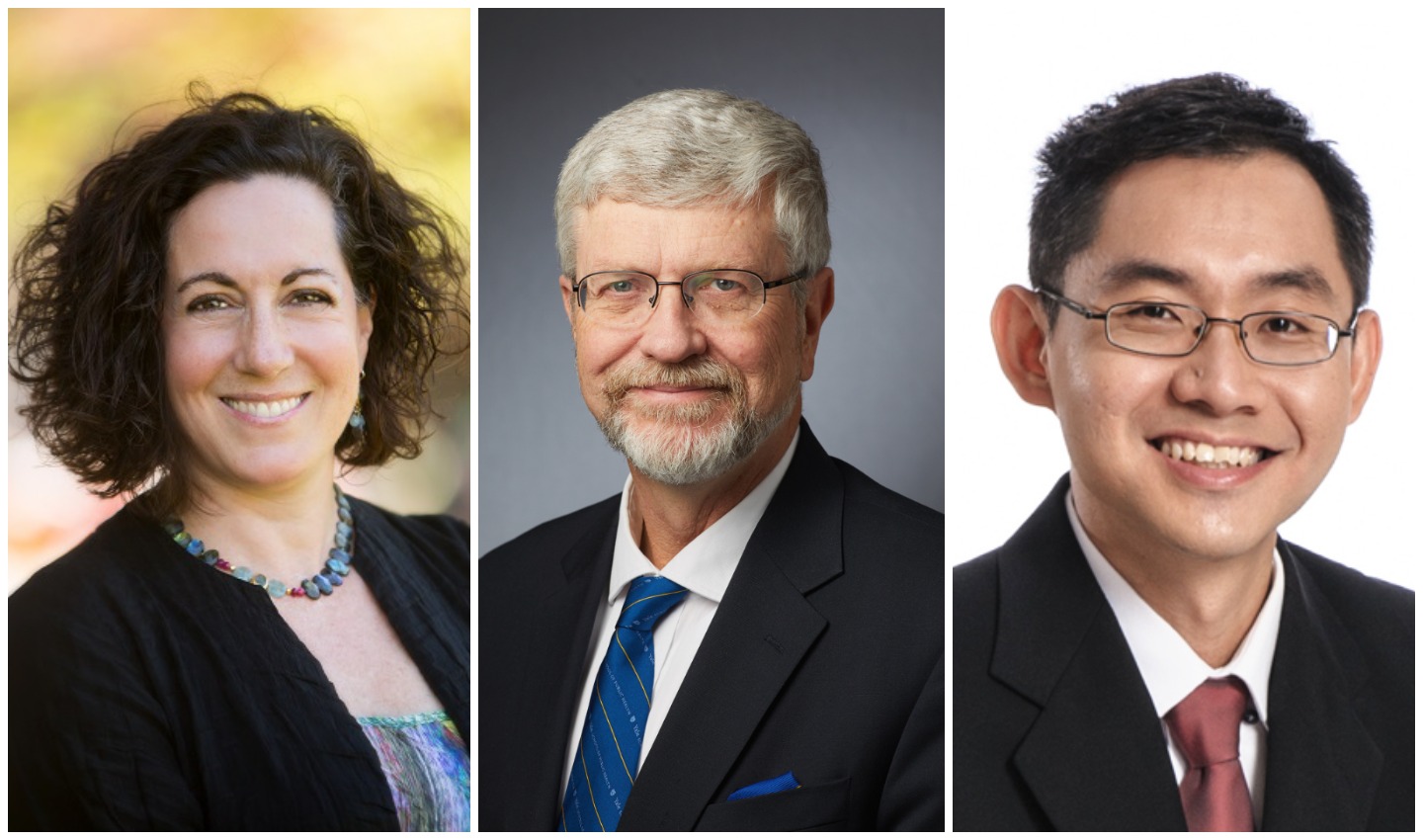 From left to right: Deans Jeannette Ickovics, Sten Vermund and Teo Yik Ying.
From left to right: Deans Jeannette Ickovics, Sten Vermund and Teo Yik Ying.
Since its outbreak in 2020, the COVID-19 pandemic has affected our lives and impacted social, economic and health conditions worldwide. We invited Yale-NUS Dean of Faculty and Professor of Social Sciences Jeannette Ickovics, National University of Singapore (NUS) Dean and Professor at Saw Swee Hock School of Public Health Teo Yik Ying and Dean and Anna M R Lauder Professor at Yale School of Public Health Sten Vermund to share some valuable insights on the challenges and future of public health, as the world grapples with the COVID-19 pandemic.
The trio will also be speaking at the “Reimaging Public Health: Global Leadership Perspectives for a Post-COVID World” webinar on Thursday, 4 February 2021 at 7pm. The event is part of a series of webinars organised by Yale-NUS College to engage its leading scholars and those from its founding institutions, Yale University and NUS, in discussions about timely topics to encourage a spirit of open conversations across the three campuses.
Singapore was better able than most countries to control the COVID-19. What are some of the lessons learned in Singapore that could be scaled-up elsewhere in the world to bring an end to this pandemic? And, what lessons might be applied in the earliest days of a future infectious disease outbreak to prevent global spread?
Dean Teo: First, Singapore is a geographically small country and there are only around seven entry points into the country whether via land, sea or air. This makes the management and control of any outbreaks logistically and operationally easier compared to other countries. However, from the very beginning, Singapore implemented a suite of public health measures that were guided by data and evidence, and these measures were reviewed regularly according to the situation locally and globally. This included comprehensive contact tracing and quarantining those infected. Second, Singapore also implemented strict border controls. Third, Singapore implemented a suite of safe management measures in the community and public spaces, and actively enforced compliance. Lastly, policy makers actively, regularly, and transparently communicated the COVID-19 situation to the public. There was a trusted source of communication to let people know what to do, how to seek help, what is the current risk of community transmission, what are the ongoing measures implemented in public to keep everyone safe – communicating these information is crucial during crisis management. These are some of the reasons why Singapore has managed to control the outbreak well. All of the above were not unique to Singapore, but were lessons that have been highlighted by the World Health Organization (WHO) during their weekly press conferences.
What can we expect as vaccines are rolled out globally? Please comment on the challenges such as vaccine hesitancy and inequities in access and distribution – as well as opportunities once vaccines are sufficiently deployed.
Dean Vermund: There are great challenges in deploying vaccines with enough coverage and fidelity to stop the pandemic. First, we have to attend to the issue of vaccine supply. Can the global biotechnological and pharmaceutical community meet the global need for billions of doses? For example, in the United States alone, only 11 million residents have been vaccinated to date, out of a population of 330 million. Second, we must address the challenge of vaccine hesitancy – many people are concerned about the safety and efficacy of the vaccines. Thus our messaging must be educational without being judgmental. Third, we have to manage the demands of logistics. We are better at giving vaccines to children but we will need to ensure that logistically, the vaccines reach the adults as well. Finally, there is the issue of cost. While high income nations are motivated to pay for the vaccines that they need, will donor nations be willing to support global distribution? Transmission can be a risk anywhere where 95 percent of the human race can visit one another in less than 48 hours of air and ground travel.
What do you think were the most important human factors that influenced the profound scale of the pandemic? What must we do to prevent the next pandemic threat?
Dean Ickovics: We are inherently a social species. Infectious disease is driven by human inter-connectedness: people together in schools and workplaces, homes and houses of worship, public transit, public parks, public protests. These months (now nearly a year) of isolation and grieving have forced us to recognise our frailties, including impacts on our physical, mental and spiritual health. We are not rational beings; judgement and decision-making are more often driven by emotions than logic. This may explain our resistance to social distancing, mask wearing and lockdowns. When we next face a global health threat, I hope that the experience of this pandemic will motivate rapid scale-up of preventive measures. We should be better equipped to anticipate questions, mobilise evidence-based interventions, and leverage the strength of human relationships to promote resilience.
You will all be sharing more about the tenets of global health now and in the future at an upcoming panel discussion on 4 February 2021. Why should our readers tune into the panel, and share a key insight you think they will gain from the session.
Dean Teo: Given the extent of pre-COVID international travel, global spread of a highly infectious pathogen appears to be almost inevitable, as we see from the Severe Acute Respiratory Syndrome (SARS) in 2003, H1N1 in 2009, and even the Middle East Respiratory Syndrome (MERS) that went beyond the Middle East to Europe and East Asia. Routine surveillance and the rapid sharing of information are two elements vital for early outbreak management. However, while these are easy to put in words, the reality is that it is extremely difficult to implement a rapid detection and response protocol even in the most well-resourced countries.
Dean Vermund: Global health has never been a more compelling paradigm than it is now. Pandemic threats are best addressed at their sources. A highly effective global health network is essential, with a strong WHO, and openness among ministries of health to share information and partner on disease prevention and control.
Dean Ickovics: Change is constant – what has been unique is the accelerated pace. We will try to address which changes are durable and why. Telemedicine, telecommunicating, remote teaching/ distance learning: it seems we won’t fully retreat to our old ways, though the balance of high technology and high touch is not yet clear. What is clear is that we must rebuild public health infrastructure and cross-sector collaboration; sustain advances in scientific discovery and innovations in clinical medicine; assure equity; nurture global partnerships and strengthen political will.
The “Reimaging Public Health: Global Leadership Perspectives for a Post-COVID World” webinar will be live-streamed on the College’s Facebook page on Thursday, 4 February 2021 at 7pm.